Health Organisation Award
This category is for organisations working effectively with consumers to improve services. The Award recognises health organisations that demonstrate an ongoing partnership with health consumers to improve health outcomes.
And the Winner is…

Pictured from left to right: Hon. Alanna Clohesy MLC, Renae Hilder, Nicole Bell, Susan Jetta, David Burns-Wallace and Jason Wolf.
Moorditj Djena
Moorditj Djena means ‘strong healthy feet’ in Noongar language. The Moorditj Djena Program is a high-risk foot and diabetes education service for Aboriginal people which focuses on prevention and management of foot complications. Patients receive podiatry, diabetes and nutritional education services at various community clinics across the metropolitan area in a combination of community venues and using a customised mobile clinic van. Many of the clinic locations are run in partnership with other agencies and stakeholders providing services to Aboriginal people, resulting in a shared care approach. The focus of the service is to identify and manage risk factors related to foot health and diabetes, initiate recall systems, and provide intervention and referrals relative to risk category.
The holistic model of care provides patients with the opportunity to talk to an Aboriginal Health Professional (AHP) as their first point of contact. The AHP conducts an initial health assessment and engages with the patient about their specific health and social needs, providing culturally appropriate referrals to other specialist health and community services as required. The patient is then referred to the Moorditj Djena Podiatrist, Diabetes Educator and/or Dietician as appropriate, for foot care treatment, diabetes education, nutrition and healthy lifestyle education and advice. The patient participates in developing a care plan with clinicians that assists them to self-manage their chronic condition/s.
 Pictured from left to right: Nicole Bell, Renae Hilder, Jessica Brimage, Susan Jetta, David Burns-Wallace,
Pictured from left to right: Nicole Bell, Renae Hilder, Jessica Brimage, Susan Jetta, David Burns-Wallace,
Brooke Blore, Gerard Lockyer and Kevin Pennington. Absent: Michelle Brassington and Shanelle Marygold.
Finalists are…
 Pictured from left to right: Lorna Cook and Julie Adams
Pictured from left to right: Lorna Cook and Julie Adams
Chemo@home
In 2013, Lorna Cook and Julie Adams started an innovative company called chemo@home.
The company administers chemotherapy for cancer patients, and many other infusions patients may have to receive for chronic illnesses such as multiple sclerosis, inflammatory bowel disease and rheumatoid arthritis, in the patients’ own home.
Since opening their doors, their highly-trained chemotherapy nurses have administered in excess of 5000 treatments to patients throughout metropolitan Perth and most recently have opened their service to patients in Adelaide. The treatments are covered by most health funds meaning no costs for private patients.
The company has received many business awards and accolades from grateful patients and their families and Lorna and Julie continue to lead the company’s growth and expansion.
 Pictured from left to right: Juanaili Hultzsch, CEO Antonella Segre, Christine Hendricks, Fiona Hughes, Georgia Booth, Amanda Muir and Danielle Kroonenburg.
Pictured from left to right: Juanaili Hultzsch, CEO Antonella Segre, Christine Hendricks, Fiona Hughes, Georgia Booth, Amanda Muir and Danielle Kroonenburg.
ConnectGroups
ConnectGroups, established in 1983, is the peak body for peer Support Groups in WA, empowering and sustaining Self Help and Support Groups (SHSGs) through resourcing, education, training, and access to small grants. Programs are developed to advance the capacity of individuals, families and carers who are actively engaged with SHSGs. SHSGs provide peer support on a wide range of issues including chronic and genetic conditions, trauma, mental health and social challenge, and to provide a referral pathway to those individuals, families and caters as an integral part of their early intervention, prevention and recovery journey.
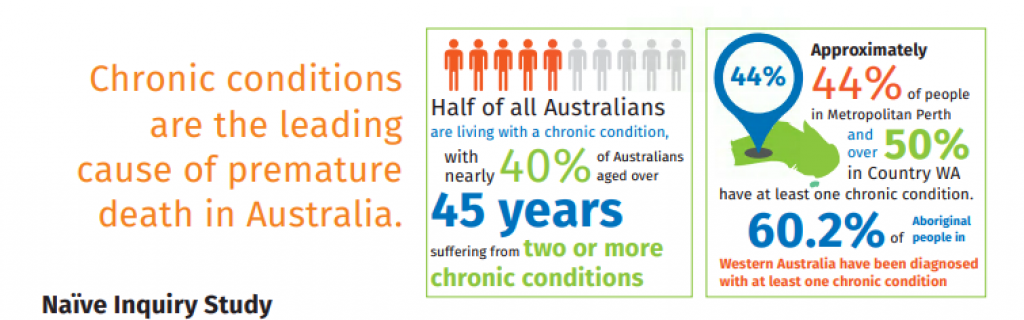
ConnectGroups’ ‘Live it Forward Together’ small grants program builds referral pathways and capacity-builds chronic conditions self-management Support Groups. The program provided funding to Support Groups and organisations for projects demonstrating sustainable chronic conditions self-management outcomes, and enabled SHSGs to provide better services, information, education and support to their members and to the wider community. An evaluation of the program demonstrated that over 2,000 individuals with chronic health conditions were impacted by the projects.

Pictured: Karen Stiles. Absent: Shannon Finucane.
Healthy, Well & Wise – Bentley Mental Health Services
The 12-week Healthy, Well and Wise program provides a combination of education, support and practical skills to Bentley clients. With cooking, exercise sessions and weight loss strategies all on the menu, the program is designed to encourage health living once clients return home.
Each week the program features a group leader, such as a dietitian, physiotherapist or psychologist, who cover different topics. The multi-disciplinary team approach ensures once the program is complete, each participant has the skills to be healthy, well and wise.