In our previous Health Matters focused on self-advocacy and peer support, Rhianwen Beresford, Convenor of the WA Peer Supporters’ Network, spoke about a vision for peer support where every Western Australian knows what peer support is and can access it if they want to.
Peer support happens across all sectors and walks of life. If you’re using your own experience to help someone through a similar experience, that’s peer support. Mental health peer support offers a whole range of benefits – friendship, empowerment, lessening of stigma, increased acceptance, and shared insights about life with mental health experiences.
On a larger scale, mental health peer support can have a positive impact on the way society views and treats mental health, leading to improvements in service and more person-centred, trauma-informed responses.
Carli Sheers is an active consumer representative and mental health advocate, and we spoke to her about the importance of peer support.
Why is mental health important to you and what made you want to become active in this space?
I recovered from mental health issues through accessing peer support many years ago, and have worked in the mental health sector in various roles for 13 years. My experience and skills as a Consumer Consultant have grown through active participation in the sector and Membership of Mental Health Australia’s National Register. With intention, I developed an extensive network of mutually beneficial collegial relationships and can speak from beyond my own personal experience with their consent. I am lucky to have access to a peer mentor who I admire, respect and value. I became active in the mental health sector to raise the expectation of recovery, reduce stigma and discrimination, and increase my employability as employment is an indicator of health. I also invested in my education and founded a mental health education and training consultancy business last year.
What are the major benefits of mental health peer support, and why does it play such an important role alongside clinical treatment options?
Peer workers undertake a variety of functions in diverse settings, from service delivery to policy making to funding of services. Personal lived experience is an essential job criterion, and other competencies include a person’s overall life experience, employment and education history, emotional maturity and ability to engage and communicate. Peer workers provide an effective and high-quality intervention that can be either complementary to clinical service or, in some situations, effective as a stand-alone intervention. They see challenges as growth and learning opportunities, not as crises.
Mental health peer support workers are experts by experience and provide a specialist knowledge base that can transform individual lives and systems of care. They are recognised for using their insights and expertise from their personal expertise to inform their work, and can walk alongside people who have experienced similar distress and support them without trying to ‘fix’ their situation. It is about engaging people with mental health issues as the central actors in their management of their mental wellbeing, helping them to find meaning in their life experiences, and guiding people’s journeys towards a contributing life. This was my experience when I accessed Grow*, a national consumer mental health organisation.
Major benefits of mental health peer support include helping people to believe in themselves and re-build their lives, discover their own solutions and develop a sense of control, master their emotional strengths, work towards self-agency and self-advocacy, enhance the quality of lifestyle and personal choices, and finding their strengths, capabilities and possibilities. Peer workers influence much needed cultural change in services and workplaces, decrease people’s need for costly acute services, and are effective in engaging people who have been difficult to reach and not benefited from traditional services.
(Source: Peer Work in Australia. A New Future for Mental Health. 2018)
In the wake of COVID-19, many people are finding themselves on a new mental health journey. As someone who advocates in this space, what advice would you give?
Navigating the mental health system can be complex, as there are many pathways for care and support. It is important to ask for help, and I encourage people to see their GP (or access a Telehealth appointment) if they are not coping due to COVID-19.
I also refer people to the WA Mental Health Commission’s website as a reliable source of information about supports and services. Consider joining a support group via ConnectGroups (https://connectgroups.org.au/), who are the peak body for support groups in WA.
Do you have any advice for those interested in becoming a mental health consumer advocate?
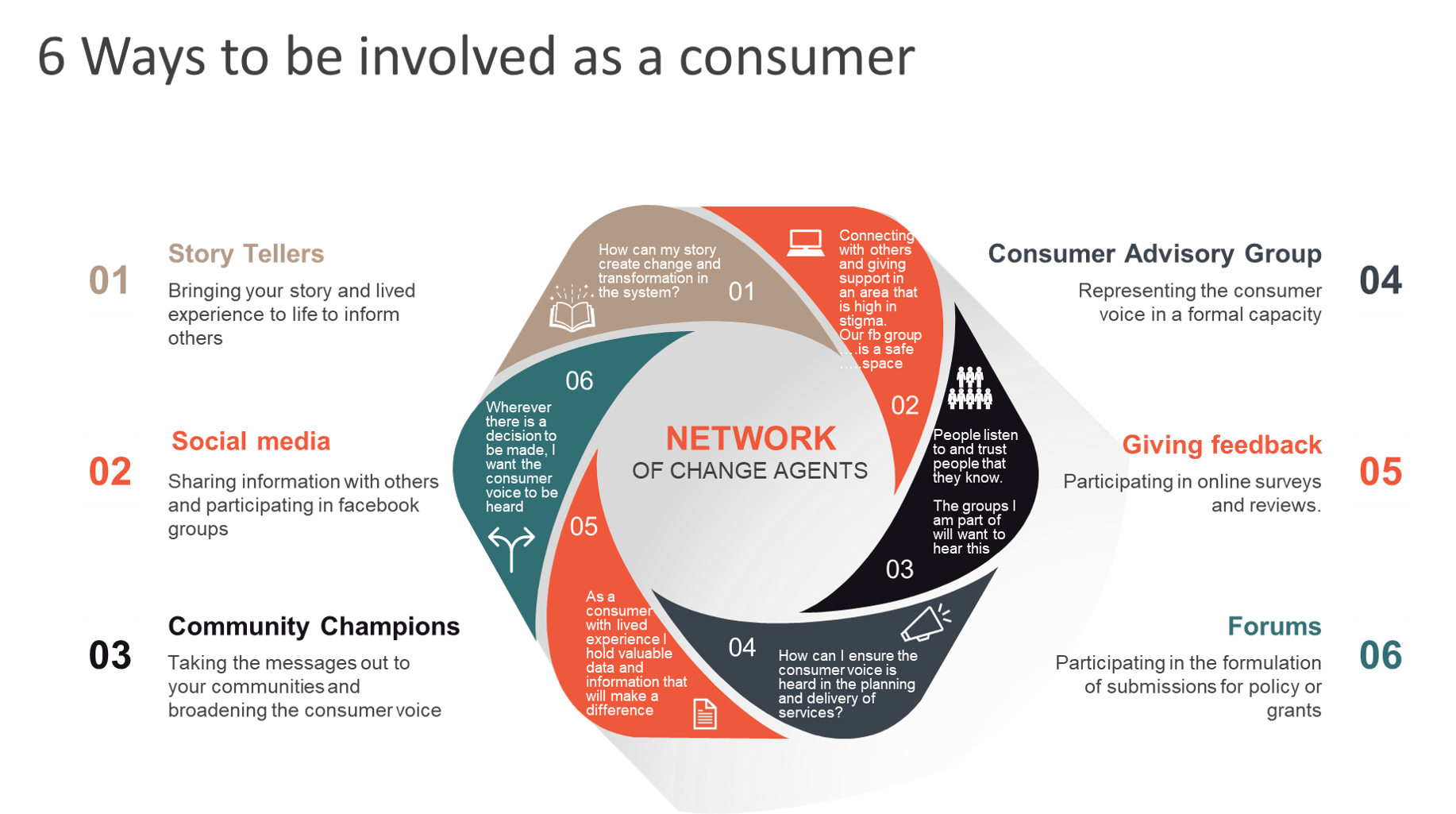
Life-long learning is important to being an effective mental health consumer advocate. I encourage people to access Consumer Representative training via Health Consumers’ Council and Consumers of Mental Health WA+.
*Grow is a community-based organisation that has helped tens of thousands of Australians recover from mental illness through a unique program of mutual support and personal development. To find out more, visit https://www.grow.org.au/
+CoMHWA currently hosts the WA Peer Supporters’ Network (WAPSN), a network for and by peer supporters in Western Australia. You can join or find out more by contacting info@peersupportwa.org.au or contact (08) 9258 8911.
This article was originally published in Health Matters