HCC’s Consumer representatives give feedback on ACHSM pre-congress workshop
Over 100 ppl — mostly health service providers — but certainly including at least 12 HCC consumer representatives, attended a pre-ACHSM* congress workshop, “The future of healthcare in Australia: designed for consumers, enabled by digital, and accessible for all” held at Perth Convention and Exhibition Centre 21-23 September 2022. Following the event, we asked our HCC consumer representatives who attend the pre-congress workshop for feedback. Read further to find out what they said.
The session was entitled “Future for healthcare in Australia: designed for consumers enabled by digital access for all’. The main presentation gave an overview of the Deloitte, Curtin Uni and CHF white paper entitled ‘Australia’s health reimagined. The journey to a connected and confident consumer.”
Noted by one consumer: the very title of the session …designed FOR, not designed WITH!
In this white paper it shows where the opinions of stakeholders lie about where the health system currently sits, as well as priorities for change.
The three “horizons” – ‘connected’, ‘empowered’ and ‘confident’ consumers – are envisaged to exist as a progressive step approach to a reimagined health system which ‘supports all Australians to live their best, healthiest lives.’ The white paper describes a number of transitions that will reorientate the health system to focus on the needs of individuals.
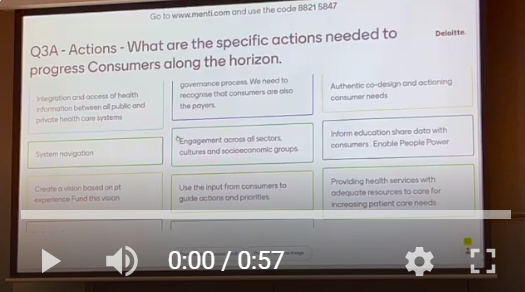
Following the review of this report’s findings, the audience was asked to participate in a series of Menti polls (Mentimeter is an online, interactive, live polling tool used to ask questions at events, and provides the audience’s responses on screen). Polling activities looked at views on the current state of healthcare and its use of digital health in terms of three horizons, connected, empowered and confident consumers.
Overall, many of our consumers suspected that that the room was not very consumer focused in its perspective.
One consumer said that when voting on priority focusses, the important dimensions to focus on that will accelerate the health system toward achieving its visions (e.g., consumers moving along the “horizon” from “connected” through to “empowered”), the dimensions relating to consumers came in as priorities 5, 8, 12 and 13. Priorities 1-4 were system funding, system integration, enabler workforce, and enabler data interoperability.
The priority responses from the room were all about the providers and the system doing things to reform itself – not starting from where consumers are and what they need.
There was a lot of academic and high-level commercial ‘report’ jargon thrown around the room, said another consumer, which is not very consumer-friendly regarding simple language or a ‘give it to me straight, doc’ approach.
One of our consumer representatives said he was “very surprised that the title suggested workshop for consumers but [that consumers] were very outnumbered by others [e.g., health service providers]”.
However, more than a couple HCC consumer representatives found the workshop to be positive and most worthwhile with a good spread of consumers in the room and plenty of opportunity to get the consumer perspective heard and captured, especially using Menti. A couple consumers mentioned Menti being useful:
“…the electronic way [using Menti] of gathering comments, opinions and insights (via phones) is an efficient way of conducting the workshop, especially when only 1.5 hours is allocated.”
The strong consumer feedback will help shape the next phase of the work.
Of interest, the point was made that health providers and clinicians are also service users and so they should look at what they would want to receive for themselves and their loved ones.
Another consumer seconded that point of view, saying “A moot point was that we are all consumers at one time or other.”
It is worth highlighting concerns of another health consumer in attendance:
“… about the comments made [regarding] ‘we are all consumers of health services’ by the group. I think it is really important for not only health service providers but also health workers and those in leadership positions across the system, to understand that being a consumer of health services means different things for different people. While I agree that we all should receive the same access to digital health tools, there needs to be a recognition of the complexity of need for consumers with complex health issues compared to those who perhaps step in and out of the health system periodically throughout their lives – and digital solutions need to address this and respond to it. People with chronic health conditions…often have contact with the health system on a weekly basis and require a more intensive, complex, and sophisticated relationship with the system, to meet their needs. I don’t believe this level of complexity is necessarily understood or appreciated by people who don’t have lived experience of chronic disease and multiple comorbidities. I think to say, ‘we are all consumers of health services’ is being blind to the varied complexities of consumer experiences and it is essential to have people living with complex chronic disease who are reliant on the health system constantly, in leadership positions in health, to ensure this is understood and provided for in digital health strategy.”
Some pointed out that if the health system did not hurry up and adopt more digital health resources then digital disruption would mean consumers met their needs elsewhere as private companies enter the field and websites such as https://www.patientslikeme.com/ are set up.
(This was echoed by another consumer who attended an event in August 2022 – read the blog here: “A wild reflection from digital health summit”.)
More quotes, and feedback:
There have been many similar strategies in the past and many of our consumers remain unconvinced that we need another one at this point. For example, many of our people specifically mentioned the National Australian Digital Health Strategy and that it involved “extensive community consultation across the country”.
…it is frustrating to see a restart, rather than building on what has been done previously.
I fear that there are many efforts to improve the health provision in the community but is it still being addressed in silos.
I would love to see a co-design committee developed to move ahead with what priorities can be worked on in this space.
There is no “one size fits all” and there are many things that need to be improved within WA Health. How can we move forward with realistic and achievable outcomes is my question?
As an aside – one health consumer recommends the 2017 Documentary “Daughters of Destiny” on Netflix and is convinced that starting health literacy awareness in early education is absolutely necessary.
[Noteworthy: October is Health Literacy Month.]
One consumer noted that “we [the attending workshop participants] were not told how the survey of approximately 1,800 people was administered nor the characteristics of the respondents.” She said, “This raises concerns about representativeness and possible bias if it was largely administered digitally as this may result in an overstatement of willingness and desire to adopt digital health resources.”
(~ Since the session she discovered it was indeed an online survey)
“A central focus on health outcomes was not explicit and evident in the presentation, and that is always a concern,” one consumer shared. “It must be the starting and end point, with the strategy articulating a pathway for delivering improvement.
Digital health is not a silver bullet and cannot be considered in isolation of the “health” ecosystem – it is an enabler along with other interdependent components that must be represented as part of a holistic solution that brings in a stronger community role and emphasis on consumer responsibility.”
“We all need the reassurance that there will be benefits of an integrated system that it is sustainable, workable, and where all [are] included [with] no one left behind…
Our regional services need aligning around Australia. Our Indigenous communities need appropriate consultation. Multicultural people need accessible info. Gender diverse, neuro divergent, and multiplicity of broad users need to be recognised and accepted as service users with their own often co existing diversity and needs. We know mental health concerns have also risen throughout Australia over past three years, not to mention our ageing population with continuing and varying need.
[Noteworthy: October is World Mental Health Month.]
If we are not delivering appropriate health care now to those in need, how do we expect anything new to be accepted, or are we going to have to supplement upcoming changes with the loss of something already existing?”
Overall, although with mixed levels, HCC consumer representatives thought the white paper is a useful contribution. However, there are several concerns that “not enough attention is paid to the digital divide either in the report or the workshop and there is a real danger it will gloss over the difficulties of access for some and rather than delivering something that is person-focused. It will assume that all consumers want and are able to access digital health and therefore replicate existing inequalities rather than break them down.”
***
Follow our social media platforms for ongoing commentary and contributions from our consumer representatives and the HCC team.