By Nadeen-Laljee Curran, mother through surrogacy in the USA
Recently the WA government accepted a series of recommendations from its Ministerial Expert Panel (MEP) on Assisted Reproductive Technology (ART) and Surrogacy laws. To say we at the Health Consumers’ Council were thrilled would be an understatement. It’s been an emotional few weeks for me, as my daughter was born via surrogacy and these changes personally affect me and friends and acquaintances in my community.
Speaking more broadly though, we are delighted to see the power of advocacy in action and common-sense prevailing. This review proposes to repeal the Human Reproductive Technology Act (which is 32 years old) and the Surrogacy Act (which is15 years old). This is necessary in our view as reproductive technology is a space which continues to be steeped in scientific advancement and innovation, and in today’s society has a much broader and more inclusive definition of family than was the accepted societal definition in the decades when these laws were created. We are an organisation with the value of equity at its core and we recognise that to date WA laws have been discriminatory and, in some areas, simply not fit for purpose, nor in line with the rest of the country.
In summary, the recommendations address issues around equity of access to reproductive technology and modernising and streamlining processes and procedures in this space. There are 46 recommendations in total and the report is complex so I have made a summary which you can read here and below is our overview and thoughts on the “big-ticket” items.
Access for all
I will start with this as this has been (arguably) the biggest issue to date. Our current law prohibits gay men in same sex partnerships, single men, transgender, non-binary and intersex people from accessing surrogacy – and in this regard is in direct violation of antidiscrimination law. To date WA’s ban has forced many people overseas to access surrogacy as the only option to biological parenthood. Going overseas, as I know firsthand, is fraught with huge challenges and financial burden, and in some instances exposes people desperate to become parents to significant legal, health, psychological, and financial risk.
The new law will make it so that people accessing Assisted Reproductive Technology (ART) must not be discriminated against on grounds which include, but are not limited to, sexual orientation, relationship status, gender identity, disability, race or religion. The proposed legislation will also use gender inclusive language. Finally!
The MEP report recommends that the change be implemented as soon as possible.
Abolition of the Reproductive Technology Council (RTC) and creation of a new regulatory structure
This is the biggest change in the way the sector will be regulated. Abolition of the RTC is something that has been discussed for a while. The new law will mean regulatory body approval will not be required for surrogacy (and other reproductive procedures) instead putting the onus on ART providers.
Some of other the positive changes include:
- No need for surrogacy arrangements to be approved. The decision-making will lie with the clinicians.
- Decisions around storage of gametes and embryos to be made between patients and licensed ART providers (without regulatory body approval in the main).
- Decisions around import and export of gametes and embryos to be made between patients and licensed ART providers (without regulatory body approval in the main).
A new advisory/review board will be established for the purpose of decision making on contentious or innovative ART procedures. We are really pleased to read that the proposed board composition will include a consumer. However, we note that the recommendation is for either a person who has used ART or is born of ART, and note that these are quite different perspectives. Ideally there would be two consumers who can work together and support one another; we will do our best to advocate further in this space to encourage the creation of a second consumer role or a deputy position.
Removal of a lot of the surrogacy red tape
Finding a surrogate in WA, and then a lengthy process with huge amounts of red tape, is cited by the report as being a reason that people go overseas – even if they are cis-gender, heterosexual, infertile people who would qualify for surrogacy in WA.
In the context of the low numbers of WA surrogacy, the MEP report notes that it is very difficult to find a surrogate in WA. Advertising is actually legal in WA (so long as it is not commercial), where it isn’t in other states. However, the review notes that knowledge of this fact is limited and that ART providers have not exercised opportunities to connect intended parents and surrogates (in our view this has been due to fear of breaching complex laws and suffering penalties). The report emphasises that ART providers can and should advertise and broker for altruistic surrogacy. The report also notes there is a strong case for community education and public awareness campaigns in this space.
The new legislation will not require regulatory body approvals for surrogacy as mentioned above, has an expanded allowance for reimbursement of surrogacy expenses and allows registered and experienced ART counsellors work with surrogacy cases (rather than just RTC approved ones). It also drops the requirement for the surrogate to have previously given birth to a live child.
Supporting donor conceived people to able to access information about their genetic heritage
The proposed legislation will make provision for a central donor register and access for donor conceived people to identifying information about their donor, regardless of when they were born. This is in line with an international shift towards recognising the interests of donor conceived people and the potential harms of being unaware of your donor conception until adulthood. HCC very much supports this.
The MEP report recommends an addendum to birth certificates noting details of donor conception (including surrogacy) and that donor conceived people be notified at 16 years of age that more information is held about them at the Office of Births Deaths and Marriages.
It should be noted that gestational surrogacy (surrogacy where there is no genetic connection between surrogate and child) is to be included in having this addendum, and has not been separated out due to no genetic linkage.

Legalising reciprocal IVF
Reciprocal IVF is where one person in a same-sex partnership contributes their egg and the other person is the carrier of the baby. This will be allowed in WA under the new law. To date, same sex (female) couples have had to choose one person to be both the biological and birth mother or go overseas to access reciprocal IVF.
Creating a route to legal parentage for those born via overseas surrogacy
This will allow the 400 plus children born overseas to WA parents since 2008 to finally have their parents recognised as their parents.
Yes, you understand correctly, the current law in WA does not recognise my biological daughter as my daughter or my husband, her biological father, as her legal father. The reason being, she was born via overseas surrogacy.
This has caused me significant psychological distress but no issues in practice, as she has citizenship by decent and is on my Medicare card, but in theory I could have difficulties with government authorities such as schools and hospitals and with inheritance rights. I have always argued this is a human rights issue as it is effectively creating an orphan (on paper). Our surrogate signed a surrogacy agreement to say she wanted to birth a child only and had no desire to parent, and then went to a Californian Court of Law to renounce any parental responsibility so she is not my daughter’s parent. If we too are not her parents, then who is?!
I wish my daughter’s American birth certificate, which states my husband and I as her parents, was accepted here but in lieu of that I cannot wait to legalise my own flesh and blood as my child and just hope the legal process doesn’t cost me too much more stress or money. I am not sure how this will work yet but I will be looking into it so I will let you know.
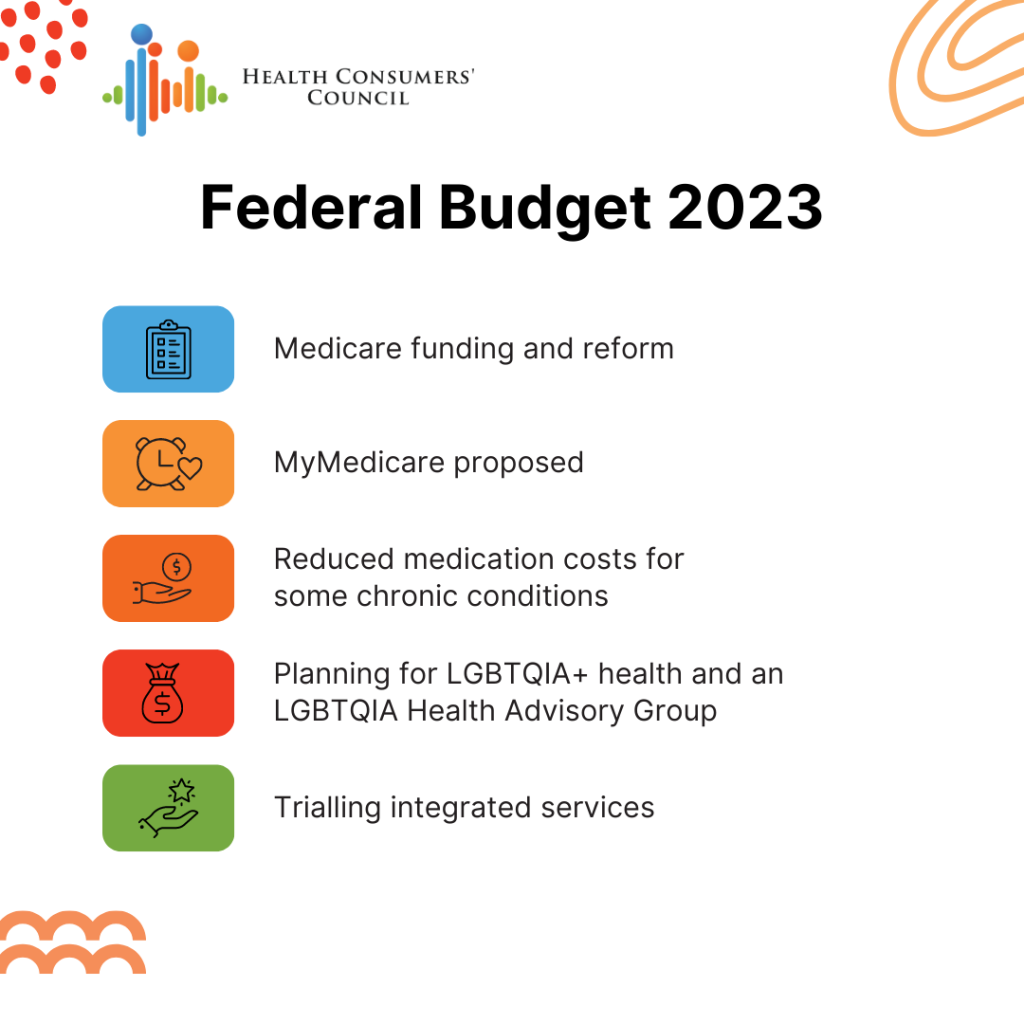
Other matters of inequity which were out of scope of the review but mentioned in this report include: support for conversations being had with the commonwealth to expand the Medicare Benefits Schedule to include IVF for surrogacy; exploring options for public IVF treatment; provision for some delegated practitioners to offer (limited) procedures in regional WA; and a recommendation that the Department of Health explore options to improve access to ART for Aboriginal people.
We are really excited about these upcoming changes and hope they will be enacted soon. We will keep you updated, so watch this space!





 use Aishwarya’s CARE Call.
use Aishwarya’s CARE Call.