Navigating change: reflections on planning, learning, and the critical need for consumer voices
By Clare Mullen, Executive Director
May is a pivotal month in our calendar year at Health Consumers’ Council. It’s the time where we finalise our plans for the next financial year (which starts in July), which means also finalising our budgets. It’s always a challenge to match our ambition for the WA community and the health consumer community with the limited resources that we have available.
We have been fortunate in the last 12 months to have received some additional funding—small amounts of short-term additional funding from the Health Department and the Mental Health Commission. But our last opportunity for any significant change in our funding was in 2014 when the health system environment – and the scale of the issues faced by health consumers – were very different.
Despite these constraints, we’re excited about what we have planned for next year. We’re very much focused on building the data and the evidence that we need to make a strong case as we hope to negotiate future funding and demonstrate the impact of the work that we are doing. We’re also looking forward to rolling out the self-advocacy workshops and resources we’ve been developing over the last few months – and thanks to those of you who worked with us on those.
Conference season: learning and sharing insights
May is also a busy time because there are lots of conferences that take place around now. I was fortunate to have been invited to put forward consumer interests in several important forums.
Primary Health Alliance Conference, Melbourne
First up, I attended the Primary Health Alliance Conference in Melbourne, where there were many conversations about how to make primary care more accessible and affordable to more people in the community. And in particular, how to enable more people to be able to access multidisciplinary care in a GP practice. I came away from that event thinking about our role in helping to build consumer and community understanding of some of the funding reforms that are needed. I’m looking forward to seeing what comes next with that.
Australian Centre For Value Based Healthcare Congress
Next, I had the chance to facilitate a panel discussion at the Australian Centre For Value Based Healthcare Conference, where we heard from one example of a co-design project that one of the consumer participants described as the best co-design project she had ever been involved with!
We also heard from New South Wales Health, where I learned about some of the data they’ve collected through their patient reported experience measures (PREMs) and patient reported outcome measures (PROMs). This has demonstrated the link that if you get the experience right for people, that can impact positively on the outcomes for people, which also impacts positively on the cost of care. This is really the essence of value-based healthcare: improving experiences, improving outcomes, and improving value for money.
You can read about some of the NSW work – including the link between dissatisfaction with food and health outcomes – here: https://www.bhi.nsw.gov.au/About_BHI/Blog/growing-evidence-on-the-link-between-patients-experiences-and-outcomes

L-R: Alison Coughlan Health Consumers Centre Vic; Anne-Marie Liddy, Chair, Health Consumers Qld; Clare Mullen, HCCWA; Susannah Morris, Consumer Leader from WA; Jessica Lamb and Kathryn Briant from Health Care Consumers Association ACT
It was also a great opportunity to connect with other consumer advocates and leaders including colleagues from Victoria, Queensland and the ACT.
At Health Consumers’ Council, we’ll be doing more work on value-based healthcare because it’s a really important concept for people who are involved as consumer representatives – particularly those at executive level and above. It’s one of the ways that we can use the work that’s being done on PROMs and PREMs in Western Australia to drive better experiences and better outcomes.
Thank you to the Australian Centre for Value-Based Healthcare for funding my travel and accommodation to enable me to participate in this and the primary care event.
Ageing Australia Conference
This week, I was invited to be part of a panel at the Ageing Australia Conference in Perth. Many of you will know that the aged care sector is going through significant reform with the implementation of the new Aged Care Act, with elements of that coming into play from 1st July 2025.
The new Aged Care Act is being billed as a rights-based act and so I highlighted the importance of making sure that, in a rights-based context, attention is paid to addressing the power imbalance that can exist between service providers and the people who use their services. This includes issues of equity and making sure that in the hurry to implement things by a certain timeframe, the needs of people who may not come from the dominant paradigm are also considered. I also highlighted the importance of independent advocacy and information from organisations who have the interest of consumers, residents, and clients at heart, including our partners at Advocare and COTA WA.
You can read more about the panel discussion in this LinkedIn post: https://www.linkedin.com/posts/ageingaustralia_the-transition-to-the-new-aged-care-act-panel-activity-7332769192443580416-Hvrl
National Safety and Quality Health Service Standards – towards the next edition
The first edition of the National Safety and Quality Health Service Standards was launched with the second edition coming in 2021. To inform the third edition the Australian Commission on Safety and Quality in Health Care hosted a meeting with the state/territory and national consumer peak organisations this month. It was a wide ranging discussion covering the whole spectrum of issues consumers face. In particular, I raised the issue of strengthening the standards to address racism in healthcare, as well as ensuring that the standards account for people’s experience as they transfer between different elements of the system.

L-R: Alison Coughlan, Vic Health Consumers Centre; Kate Gorman, Health Care Consumers Assn ACT; Clare Mullen, HCCWA; on screen Ellen MacDonald, Health Consumers Tasmania; Anna Flynn, Director Partnering with Consumers, ACSQHC; Naomi Poole, Naomi Poole, Executive Director Strategy and Innovation, ACSQHC; Elizabeth Deveny, CHF; seated Broni Smith, Program Manager, Partnering with Consumers, ACSQHC; Anthony Brown, Health Consumers NSW; Anna Thornton, Chief Nursing Officer, ACSQHC; Gillian Giles, Director Clinical Governance, ACSQHC; Joanne Taylor, Program Manager Comprehensive Care; Keith Tracey-Patte, Health Consumers Queensland
A system in transformation
There are changes happening in primary care, in hospital care, and in private care. At the same time, as I’ve said there is significant change happening in the disability sector as well as the aged care sector.
There are many wonderful people working in health services, in aged care and in disability services, and many of them very much have the interest of consumers in mind. But no one experiences the system as a whole other than the consumers who are trying to navigate the complexity of those various systems and how they interact – or don’t!
Never has it been more important that there are confident, connected, informed consumer representatives who are able and feel supported to speak up for the rights of consumers, carers, community members, and people with lived experience, in every room where ideas are being discussed, and decisions are being made that impact on the experiences and outcomes that people will have.
A Call to Action
If you have been thinking about whether or not you might want to draw on your lived experience or become involved as a consumer representative, I urge you to think about it now. Now is the time.
It is imperative that we have strong, confident people in the community who are coming from an informed and supportive consumer movement —where people draw on their own experience and can also put forward a broad consumer perspective. We need to be in every room where discussions are happening.
Systemic advocacy: protecting consumer rights
Consumer rights in dental care
This month has also been very busy on the systemic advocacy front. Some of you have seen the news items from The West Australian about consumers who have been left out of pocket and without dental care: https://thewest.com.au/news/health/patients-of-perth-dental-rooms-dentist-david-hurst-left-in-financial-limbo-and-pain-after-practice-collapses-c-18454547
Unfortunately, what the stories have highlighted is that there are many gaps in the system that is supposed to protect us as we access dental care. Many people are facing aggressive marketing tactics from dental companies who are encouraging people to access their superannuation in order to have dental treatment. It’s not clear whether or not people understand all of the implications of that, both for their future financial security but also for the day-to-day reality—for example, having to pay tax on super accessed early.
I will be meeting with WA’s Chief Dental Officer and the head of the Australian Dental Board next week to discuss this, and we’ll be putting forward our concerns to make sure that the loopholes that seem to be undermine the rights that patients and consumers have are closed. We want to ensure that consumers can be making informed choices in the confidence that the system that is there to protect them is working as it should.
We have a survey for people who might want to share their stories, and you can find that here: https://forms.office.com/r/WttmCBkJUd
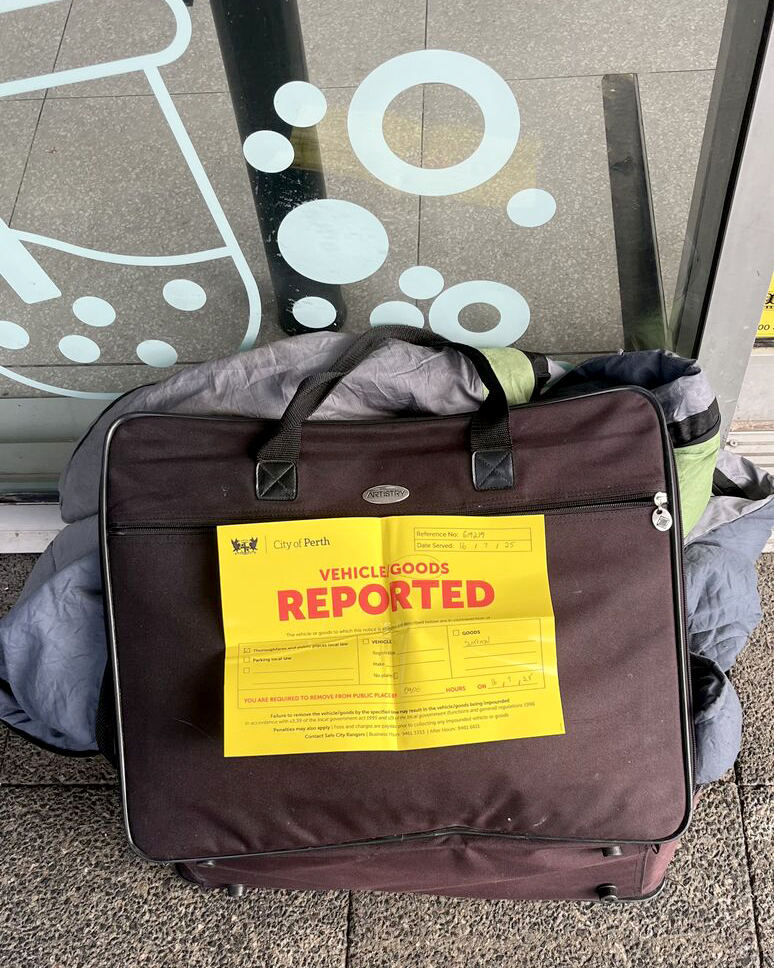
Hospital Parking: A Barrier to Care
On another front, we had the opportunity to take part in an ABC Life Matters conversation this month talking about the impact of the high cost of parking at some public hospitals. We heard about the economic argument that there is evidence showing that if family and friends are able to spend time with their loved ones while in hospital, this can help the healing process and in some cases help people get home sooner.
In Western Australia, we put a call out to our networks to understand the impact of hospital parking costs, and we know that today, right now, there are people taking out payday loans in order to access essential healthcare, including attending emergency departments.
There have been many attempts in the past to raise the issue of parking costs, and to date, those have been largely unsuccessful. There are some concessions that are available, and you can see what we have been able to find out about those on our website. But by and large, the cost of hospital parking is still a barrier to care for many people.
The reason that we are taking up this issue again is that having spent a state election period hearing about how we are the state with the strongest economy in Australia we think that the stark contrast between that and the reality of people trying to access healthcare is really quite stark.
We’ve raised this already with the new health ministerial team, and we also reiterated it in our budget paper that we submitted to the ministers last week. Again, we have a survey inviting people to share information about their parking experiences. We won’t share any details that identify anyone, but as we know, lived experience stories can change minds and hearts. So please, if you have a story to share, please do—here’s the link: https://forms.office.com/r/NFq9WhFcKM
Advocacy in Action: Meeting Growing Community Need
Finally, we have been very busy in both our engagement team and our individual advocacy team. What we identified is that in January to March 2025, compared to January to March 2024, our individual advocacy team saw an increase in the number of priority cases that far exceeded 500 percent—more than a five-fold increase in the number of priority cases.
Every case is important, but for example, if you are in hospital right now and reaching out to an independent advocate might be able to help you in that particular situation, then we will do our best to support that person as quickly as possible.
As Health Consumers’ Council is the only state-based consumer organisation in Australia that provides independent individual health advocacy across the whole range of health issues—mental health, physical health, primary care, hospital care, private healthcare, and public healthcare (the only area that we don’t cover is involuntary mental health)—this increase is significant.
What is curious to me is why health advocacy is so poorly resourced compared to advocacy in the disability sector and advocacy in the aged care sector. Advocacy is much needed in any sector where public services, just by the way they exist, are difficult for people to navigate. You need people who understand those systems to walk alongside you and support you as you stand up for and defend your rights and seek redress when things have gone wrong.
A big piece of our advocacy is continuing to advocate for more access for the community to independent health advocacy across all areas of health.
Engagement and Innovation
In our engagement team, we have had a whole range of events take place this month. We gathered together consumer representatives from across the healthcare system to understand how Care Opinion is being used in their health service and what opportunities they saw as consumer reps for using it differently. We have a few ideas that have emerged from that, so watch this space. We’ll be hosting another conversation with that same group alongside the staff who work on Care Opinion later in the year.
This is thanks to a small amount of funding that we got from the Health Department to progress work in relation to Sustainable Health Review Recommendation 4, which relates to the objective of expanding the use of Care Opinion.
The other exciting news is that we are making progress to support the Health Department as they implement their safety and quality strategy. One of the strands in that work is looking at consumer leadership, and so we are initiating that work by hearing from consumers about their experience of consumer leadership. What does it mean to you? What can make it work really well, and what can get in the way of it? Again, we have a survey for that: https://forms.office.com/r/gjNuHJuNUy
Looking forward
If you’re still reading, then you’ll know it’s been a busy time. There are lots of opportunities for people to influence change in the system. If you have ideas for areas that we’re not across, we are a small team, but we will add it to the list of things and do what we can to support you in the community to make change for the good of health consumers, families, carers, and people with lived experience in the community.
Thank you to those of you who go above and beyond, who speak up, who draw on your own lived experience and your knowledge of the healthcare system to advocate for positive change. Never has it been more needed for us to have strong independent consumer partners to work alongside those change agents in the health system to bring about a transformed health and medical care system for the WA community.